What you’ll learn:
- Women are more likely to experience digestive side effects from metformin, especially in the early weeks, but these often improve with time and the right strategies.
- Metformin may offer unique benefits for women, including improved insulin sensitivity, fertility support, and even reduced cardiovascular risk.
- Hormonal shifts and biological differences can influence how metformin works, so adjusting your plan with your provider is important.
Let’s talk about metformin—and more specifically, what it’s like to be a woman taking it. Whether you were prescribed it to manage type 2 diabetes or to support weight-related concerns, you’ve likely heard about its benefits. These include its ability to lower blood sugar, improve how your body uses insulin, and, in some cases, support modest weight loss. It’s also widely used because it’s affordable and has a long track record of safety.
But what’s often left out of the conversation is that the experience of taking metformin isn’t the same for everyone. Research shows that women are more likely than men to report gastrointestinal (GI) side effects, especially in the early weeks of treatment.
At the same time, studies suggest that women may experience unique benefits, too. Some show greater improvements in blood sugar and insulin response, reduced cardiovascular risk, musculoskeletal pain relief, and, for those with PCOS (polycystic ovarian syndrome), hormonal regulation and potentially improved fertility.
This guide focuses on that experience: what women commonly report, when side effects tend to show up, and what can help you manage them.
The most common side effects of metformin
There isn’t any official difference in the adverse side effects that females experience vs. males. The most common side effects of metformin remain the same and include:
- Diarrhea: This is the most commonly reported side effect of metformin.
- Nausea: It typically begins in the early days of treatment but tends to ease as your body adjusts to metformin.
- Stomach pain or cramping: These symptoms may occur, especially if metformin is taken on an empty stomach.
- Gas and bloating: These are common digestive side effects but are usually mild and temporary.
- Metallic taste in the mouth: While less common, some people report a metallic or bitter taste after taking metformin.
Your dose will be increased gradually to minimize side effects while maximizing results. Learn more about how to find the right dosage of metformin.
What do women report about the side effects of metformin
Metformin can be helpful for managing insulin resistance, PCOS, or type 2 diabetes. But some studies show that it affects women differently from men. Research backs that up: women tend to report more side effects, but also some unique benefits.
- GI side effects can be intensified: Women are more likely to experience GI symptoms like nausea, bloating, or diarrhea during the first few weeks of metformin treatment. In one study, about 34% of women reported digestive symptoms just two weeks into treatment, compared to 25% of men. Because of this, women often end up on lower doses over time.
- Menstrual cycle could change: Some women also notice changes to their cycle while on metformin, especially those with PCOS. That’s because metformin can help regulate hormones that play a big role in ovulation and menstrual timing.
- It could boost fertility: Studies show it can help improve ovulation and even boost chances of pregnancy for people trying to conceive.
- It could boost mood or sex drive: Some women also report a mood boost or increased sex drive while taking metformin for PCOS, possibly due to improved hormonal balance and emotional well-being.
- Other benefits of metformin: And it’s not just hormone-related symptoms. Metformin may offer other benefits, too.
- Fewer heart issues: In one large study, women taking metformin had fewer cardiovascular issues over time than men.
- Joint pain improvement: There’s also some early evidence that women may feel more relief from muscle or joint pain on metformin, possibly due to differences in how it affects inflammation and tissue repair, though more research is needed.
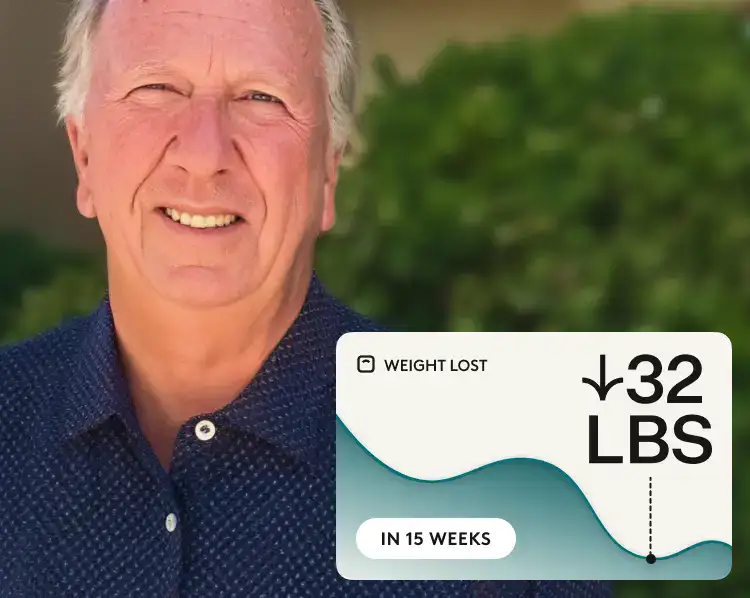
Rx weight loss, the right way, with Noom
Get access to prescription weight loss medication with Noom.Why metformin can lead to different side effects in women
Metformin works the same way in everyone. It helps lower the amount of sugar your liver produces, improves how your cells respond to insulin, and slows the absorption of glucose after meals. But even though the mechanism is the same, how it feels can vary, and women often have a different experience.
- Hormonal influences: Shifts in estrogen and progesterone—whether from your monthly cycle, perimenopause, or menopause—can change how your body processes medications. These hormonal fluctuations may help explain why women are more likely to report side effects like nausea, bloating, and diarrhea in the first weeks of taking metformin.
- Stronger glucose response: Some studies suggest that women respond more strongly to metformin when it comes to blood sugar control. One review found that women had greater improvements in fasting glucose and insulin secretion than men, especially after meals. While this sounds like a good thing (and often is), a bigger physiological response could also mean a greater chance of side effects.
- Differences in metabolism and body composition: Women tend to have slower gut transit time, different fat distribution, and variations in liver and kidney function compared to men. All of these factors may affect how metformin is absorbed and how long it stays active in the body, which could contribute to both side effects and benefits.
Together, these biological differences might mean that women may need a more personalized approach to dosing and symptom management.
Tips for managing metformin side effects for women and men
Side effects aren’t always predictable, but they’re often manageable with a few practical tweaks. Many women find that symptoms like nausea, fatigue, or cycle changes show up early, especially if they’re new to metformin or navigating hormonal shifts like PCOS or menopause. Here’s what can help ease the transition and keep your treatment on track:
- Take metformin with food: One of the simplest ways to reduce nausea and stomach upset is to take metformin with meals. Pair it with something bland or starchy, like rice or toast, to buffer the digestive effects. If side effects persist, ask your provider whether extended-release (ER) metformin might be a better fit; it’s been shown to significantly reduce gastrointestinal symptoms.
- Watch your diet, especially fats and sugars: Foods high in saturated fat or added sugar can make metformin harder to tolerate and reduce its effectiveness. A balanced, lower-glycemic diet not only supports blood sugar control but may help lessen GI symptoms. Here’s a breakdown of foods to avoid with metformin to help guide your choices.
- Keep alcohol in check: Drinking occasionally is usually okay, but regular or heavy drinking raises your risk for GI issues, and in rare cases, lactic acidosis. Here’s what to know about alcohol and metformin if it’s part of your lifestyle.
- Pay attention to fatigue and nutrient levels: Metformin can lead to vitamin B12 deficiency over time—even in the low-normal range—which can cause lingering fatigue or brain fog. Some women may also be more prone to low iron due to cycle irregularities. If tiredness sticks around, ask your provider about checking B12 and iron levels.
- Move gently, eat consistently: Regular movement—like walking or yoga—can ease digestive sluggishness and help with insulin sensitivity. And don’t skip meals, especially if your blood sugar tends to dip. Balanced eating supports both your energy and metformin’s effects.
- Track menstrual changes: If you’re using metformin for PCOS, it may help regulate your cycle and support ovulation. Any changes in bleeding, especially if unexpected or disruptive, should be discussed with your doctor.
Most side effects ease within a few weeks, especially with the right strategies in place. If something feels off or continues to interfere with daily life, bring it up with your provider—they can help adjust your dose, timing, or formulation so metformin works with your body, not against it.
Severe side effects and warnings for metformin
Most people, men and women, tolerate metformin well, especially when it’s taken as prescribed and monitored regularly. But like any medication, there are rare but serious risks to be aware of. While these side effects are uncommon, it’s important to recognize them early and get medical help if needed.
- Lactic acidosis: This is the most serious potential side effect of metformin, but it’s extremely rare. It happens when too much lactic acid builds up in the body, which can become life-threatening if not treated promptly. Symptoms may include deep or rapid breathing, ongoing nausea, abdominal pain, fatigue, or muscle aches. Lactic acidosis is more likely to occur in people with kidney or liver problems, those who are dehydrated, or those who drink heavily. Notably, studies show the overall risk is very low, with no clear evidence that women are more affected than men.
- Severe digestive issues: Mild gastrointestinal side effects like bloating or nausea are common early on, especially in women. But persistent vomiting, diarrhea, or abdominal pain could be a sign that your body isn’t tolerating the medication well or that something more serious is going on. If symptoms don’t improve, reach out to your provider.
- Extreme fatigue or muscle weakness: Sudden or worsening fatigue may suggest your body isn’t tolerating metformin well, especially when paired with other symptoms like shortness of breath or muscle pain. While women are more likely to report early fatigue, no studies suggest they’re at higher risk of dangerous reactions.
- Vitamin B12 deficiency: Long-term use of metformin has been linked to lower levels of vitamin B12 in some people. This can lead to symptoms like tiredness, weakness, or tingling in the hands and feet. The risk appears to be related to how long you’ve been taking metformin, not your sex.
- Low blood sugar (hypoglycemia): Metformin by itself rarely causes low blood sugar. However, if it’s combined with insulin or certain diabetes drugs, it can increase the risk. Watch for signs like dizziness, sweating, shaking, blurred vision, or a racing heart. Your provider may adjust your other medications to help reduce this risk.
While serious side effects are uncommon and not more frequent in women overall, keeping an open line of communication with your provider is key, especially if you’re sick, fasting, or notice anything that feels off. Regular check-ins and bloodwork can help catch small issues before they become bigger ones.
Who shouldn’t take metformin
Metformin is safe and effective for many people, but it’s not right for everyone. And for women, there may be times—like during pregnancy, menopause, or while managing other hormone-related conditions—when it’s especially important to stay alert to how your body is responding. Certain health conditions or life changes can raise the risk of side effects, so it’s always worth checking in with your provider to make sure metformin still fits your needs.
When metformin may not be recommended:
- Advanced kidney disease: Since metformin is cleared through the kidneys, reduced kidney function raises the risk of lactic acidosis—a rare but serious complication. Your provider will likely check your kidney function with a blood test before prescribing.
- Liver problems: Liver dysfunction can interfere with how your body processes metformin and may increase the risk of side effects.
- Severe dehydration or infection: If you’re sick with vomiting, diarrhea, or a high fever, your provider may suggest pausing metformin temporarily to prevent complications.
Important considerations for women:
- Pregnancy and breastfeeding: Metformin is sometimes continued during pregnancy—especially for PCOS or gestational diabetes—but this should always be discussed with your doctor. The same goes for breastfeeding, where research is ongoing.
- Trying to conceive: If you’re not using metformin for PCOS, some providers recommend stopping it a few months before trying to get pregnant.
- PCOS-specific needs: Metformin is still commonly used to treat insulin resistance and irregular cycles in PCOS, but if your symptoms change—say, after menopause or with shifts in your lifestyle—it’s a good idea to revisit your treatment plan with your provider.
If any of these situations apply to you—or if your health goals or hormonal profile have changed—it’s a good idea to check in with your provider. A quick conversation can help you stay ahead of potential issues and ensure you’re getting the most benefit from your treatment.
What can happen to women when they stop taking metformin
Whether you’ve been on metformin for type 2 diabetes, PCOS, or weight support, stopping it can come with some noticeable changes, especially for women. Here’s what the research shows:
- Weight gain and appetite shifts: Metformin is often linked with modest weight loss or appetite control, but some women notice the opposite after stopping. One study found that both weight and hunger levels tended to creep up within months of stopping metformin, particularly in people who had been on it for a shorter period of time.
- Menstrual cycle changes: For women with PCOS, metformin can help regulate menstrual cycles by improving insulin sensitivity and hormone balance. But after stopping the medication, those improvements can fade. In one study, women who discontinued metformin had fewer periods over a six-month period and showed signs of rising androgen levels..
If you start noticing weight gain, cycle irregularities, or other unexpected changes after coming off metformin, it’s worth checking in with your provider. They can help determine whether it’s a rebound effect, something else is going on, or if another treatment approach might be a better fit.
Comparing side effects: Metformin vs. GLP-1 medications
Metformin and GLP-1 medications like Ozempic® and Wegovy® are both used to manage blood sugar and support weight loss, but they work in different ways.
- Metformin mainly works in the liver, helping your body release less sugar and use insulin more effectively.
- GLP-1s work in the gut and pancreas. They’re part of a group of hormones called incretins and help your body make more insulin, but only when your blood sugar is high.
Both types of medication can cause digestive side effects, and studies show women tend to report these more often than men.
Here’s what the research shows:
- With metformin: Studies suggest that women are more likely to report side effects like nausea, bloating, and diarrhea—even at lower doses—suggesting a higher sensitivity.
- With GLP-1s: Research shows women consistently make up the majority of adverse event reports, especially when it comes to GI issues like nausea and vomiting. This pattern likely reflects a combination of biological differences and greater usage among women for weight loss purposes.
Navigating metformin: How to personalize the approach
Metformin is a trusted, affordable medication with a strong safety profile, but women can have a different experience taking it than men. Research shows that women may be more prone to digestive side effects, fatigue, and menstrual changes. At the same time, studies suggest that women may also see unique benefits, including improved insulin response, reduced cardiovascular risk, and better hormonal regulation.
Because women often respond differently, slowing down the dose increase may help minimize side effects while still delivering the intended benefits. Tracking changes in energy, digestion, and menstrual cycles can also offer helpful insight into how your body is adjusting—and whether your treatment plan needs to shift.
If you want to know if metformin is right for you, see if you qualify for Noom Med. You’ll be connected with a clinician who can see if it’s right for you and prescribe it if needed. Then, you’ll get expert coaching and personalized tools to help you build lasting habits.
Note: Metformin, Ozempic®, Mounjaro®, and Rybelsus® are not FDA-approved for treating obesity or weight loss.
Why you can trust us
At Noom, we’re committed to providing health information that’s grounded in reliable science and expert review. Our content is created with the support of qualified professionals and based on well-established research from trusted medical and scientific organizations. Learn more about the experts behind our content on our Health Expert Team page.





















 Noom Team
Noom Team
 Shoshana Fishbein
Shoshana Fishbein



