What you’ll learn:
- Lower levels of estrogen during menopause can cause physical changes to a section of the vaginal area called the labia minora.
- HRT in the form of topical estrogen is the most effective treatment for labia minora thinning and other physical changes to vagina tissues.
- A combination of medical treatments and lifestyle adjustments can significantly improve GSM symptoms and overall comfort during this period of life.
You’ve probably heard that menopause can come with issues like hot flashes, memory issues, like brain fog, and even more frequent urinary tract infections (UTIs). But the fluctuation in hormones can also change the way your vagina looks and feels.
Women’s health experts and influencers have been talking about this lesser-known effect of menopause on social media. As hormone levels change and ultimately drop, the labia minora, a part of the vulva, and the vagina can shrink to the point of almost disappearing. While of course you don’t actually “lose” them, this change can be jarring and even scary to think about.
The labia minora (the two inner skin folds around the opening of the vagina) can lose some of their plumpness and fullness. When the skin is much thinner than it used to be, it can also appear smaller. That’s why some people say their labia minora disappear or shrink during and after menopause.
Genitourinary syndrome of menopause (GSM) is the umbrella term for the full spectrum of genital, urinary, and sexual symptoms that happen when there is a major decrease in estrogen during menopause. GSM includes atrophy, a.k.a. the thinning of the vulva and vagina.
One study of postmenopausal women found that up to 90% showed signs of thinning in the vulva or vaginal area. And these changes go far beyond appearance. Thinning tissues can lead to discomfort, pain during sex, increased risk of infection, and a noticeable impact on quality of life.
We’ll go through why you might experience labia minora changes during menopause and when to expect them. Then we’ll compare different treatment options, like vaginal estradiol and other forms of HRT. We’ll also talk about whether lifestyle changes can help.
Understanding what happens to the labia minora during menopause
If you’re asking: What are the labia minora? Here’s a quick biology lesson.
The labia minora are the inner folds of skin that are part of the vulva, which is the term for all the external parts of the female genital area. The vulva includes the outer lips (labia majora), inner lips (labia minora), the clitoris, and the openings to the vagina and urethra (where urine comes out).
The labia minora sit inside the outer lips and stretch down from the clitoris, surrounding the vaginal and urethral openings. These delicate folds help protect the inner vulva from irritation, dryness, and infection. They also respond to touch and arousal, playing a role in lubrication and sexual sensation.
When women go through menopause, their bodies start producing much less estrogen. And that shift has a big impact on the vulva and vagina.
With less estrogen, the tissues of the vulva—including the labia minora—and the vagina can become thinner, drier, and less elastic. The labia minora may lose their fullness and, in some cases, become so small that they seem to “disappear.”
These changes are part of a process called vulvovaginal atrophy, which refers to the natural thinning and drying of these tissues as hormone levels decline.
When does labia minora thinning happen during menopause?
Labia minora thinning is one of several physical changes that can occur as estrogen levels decline during menopause. While often overlooked, these changes typically happen gradually and can start earlier than many expect. Here’s a look at when thinning and other vulvovaginal symptoms are most likely to appear, based on your stage of menopause:
- Perimenopause: During this stage, which typically begins in your late 30s or 40s, hormone levels fluctuate, and changes to your vulva and vagina can begin. 19% of women aged 40 to 45 report early signs of vulvovaginal atrophy, which can include labial changes.
- Menopause: This phase officially begins when you haven’t had a period for 12 consecutive months. The average age of menopause in the U.S. is 51.
- Postmenopause: Rates rise sharply after menopause, with vulvovaginal atrophy affecting:
What changes to the vaginal area and labia minora can happen during menopause?
As estrogen levels drop during menopause, it’s common to notice changes in the look, feel, and function of your vaginal and vulvar tissues—including the labia minora. These shifts can affect everything from moisture and elasticity to how the area feels during daily life or intimacy.
Here are some of the most common changes:
- Shrinkage: Lower estrogen levels can cause the labia minora (inner lips) to become thinner, smaller, or even appear to “disappear” as they lose volume and elasticity. The labia majora (outer lips) may also lose fat and tone, making them look flatter or looser. Even the clitoris can shrink slightly and become less prominent over time. One study notes that these changes are tied to loss of tissue structure and decreased blood flow.
- Dryness: Vaginal and vulvar dryness is one of the most common menopause symptoms. With less natural lubrication, the area may feel dry or tight—especially during sex—leading to discomfort, irritation, or pain.
- Increased risk of infection: Estrogen helps maintain the vagina’s natural acidic pH and a healthy balance of bacteria. When levels drop, the environment becomes more alkaline, which can disrupt the microbiome and make infections (like UTIs or vaginal infections) more likely.
- Reduced pelvic support: Estrogen also supports the muscles and tissues that hold your pelvic organs in place. When those tissues weaken, it can lead to pelvic organ prolapse—when organs like the bladder or uterus start to shift or press downward.
“The widespread impact when you lose estrogen leads to many bothersome symptoms,” says Dr. Karen Mann, Noom Medical Director and menopause expert. “The tissue in your vulva and vagina is so used to estrogen that when it is depleted, the tissue loses the ability to maintain, repair, lubricate, and protect itself. That’s why people see and feel that they “lose” their labia minora during menopause.”
What does losing the labia minora during menopause feel like?
While you may not notice your labia minora shrinking, you might notice some other symptoms. A thinner, drier labia is more fragile. The area could be more likely to tear due to sexual activity or even from clothing. These microtears can cause pain, bleeding, and irritation. Your tissues might also be more prone to infections.
In a survey of over 3,000 postmenopausal women, 55% reported dryness, 44% reported painful sex, and 37% reported irritation.
These changes to the vagina and vulva also significantly impacted their lives:
- It reduced sexual enjoyment in over half, with 59% noting an impact.
- It affected sleep: Almost a quarter (24%) had trouble sleeping due to these issues.
- It decreased overall well-being: 23% found these changes impacted their general enjoyment of life, and another 23% said it affected their mood.
These numbers highlight why women deserve better care to help not just their labia from shrinking, but to feel better overall.
When to see a doctor for labia minora thinning during menopause
For women experiencing any of these changes or symptoms, it’s important to have an open and honest discussion with a doctor or healthcare provider. These are common and important medical concerns to bring up, even if it may feel uncomfortable to discuss. The sooner you initiate the conversation, the sooner you can find effective, evidence-based treatment options to improve your comfort and quality of life.
Warning signs that you need to see a doctor sooner for immediate attention include:
- Discoloration: Areas of skin that appear lighter, darker, red, or pink.
- Abnormal growths: This can be a bump or lump that is red, pink, or white with a rough or raw texture.
- Unexpected bleeding
- A persistent open sore (one that lasts a month or longer).
How HRT can help with labia minora issues during menopause
There are two main types of hormone replacement therapy (HRT): local (also called vaginal or topical) and systemic. Each works differently in the body and is used for different menopause symptoms.
- Local HRT is applied directly to the vaginal area—typically as a cream, ring, or tablet—and is usually the first line of treatment for genitourinary syndrome of menopause (GSM). This includes symptoms like vaginal dryness, burning, and thinning of the labia minora.
- Systemic HRT, delivered through pills, patches, sprays, or gels, affects the whole body and is typically used to treat more widespread symptoms like hot flashes, night sweats, and mood changes.
Let’s break down how each one can help.
Estradiol for labia minora thinning (Local HRT)
Low-dose vaginal estrogen—most commonly in the form of estradiol cream—directly treats thinning tissues caused by the drop in estrogen during menopause. It works by restoring local estrogen levels to make vaginal and vulvar tissues thicker, more elastic, and better hydrated.
- Minimal absorption: Because it’s applied locally, only a tiny amount enters the bloodstream—meaning fewer systemic side effects.
- Tissue benefits: It boosts blood flow, supports tissue rebuilding, and helps normalize vaginal pH, which can also reduce the risk of UTIs.
This type of HRT is often recommended when symptoms are limited to the vaginal and vulvar area, like labia minora shrinkage or discomfort during sex.
Systemic HRT for menopause symptoms
If you’re experiencing both GSM symptoms and body-wide menopause symptoms, like hot flashes or sleep disruption, your doctor may recommend systemic HRT. This includes oral tablets, transdermal patches, and sprays that circulate estrogen throughout the body.
While systemic HRT can also support vaginal tissues, it’s not usually the first choice for GSM alone. Combining systemic and local HRT is sometimes appropriate when GSM is just one part of a bigger picture.
Is it safe to use HRT for menopause symptoms?
Safety concerns around HRT—especially the risk of breast cancer—were largely based on outdated interpretations of early research. More recent studies show that for women who start HRT near menopause and before age 60, the benefits generally outweigh the risks.
And when it comes to vaginal estrogen specifically, the safety profile is even stronger.
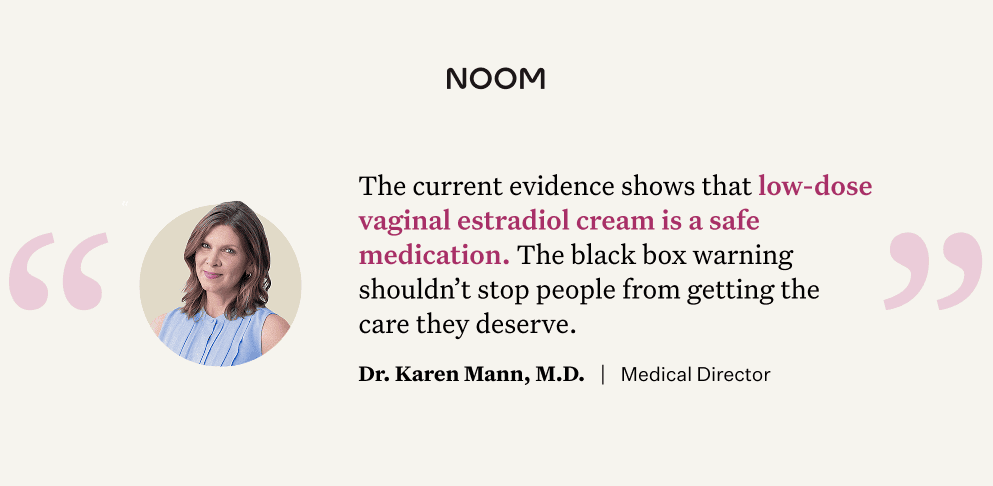
“Even though vaginal estrogen cream contains a black box warning, the current evidence shows that low-dose estradiol is a safe medication. There is debate over whether to get rid of this warning because the science over the past 20+ years continues to prove the warning is likely not needed. I want people to know that the data is on our side and the black box designation shouldn’t stop people from getting the care they deserve,” says Dr. Mann.
The key to safe HRT use is a personalized approach, where your doctor considers your age, health history, and specific needs.
Lifestyle adjustments you can make to manage vaginal health during menopause
Broader lifestyle choices and behavioral interventions may play a significant role in managing GSM symptoms and promoting overall vaginal health. Just don’t expect them to work as well as HRT.
“Self-care measures, such as avoiding smoking, ensuring adequate sleep, and avoiding vulvovaginal irritants, are helpful,” says Dr. Mann. “Though these practices are crucial for health, they don’t inherently replace the hormonal shifts that lead to difficult symptoms.”
Here are some ways you can manage your vaginal and urinary health after menopause, though they cannot prevent GSM alone:
- Use moisturizers: Used a few times a week, they help restore moisture and elasticity by adhering to the vaginal lining and encouraging natural lubrication. They’re especially helpful for easing dryness and mild discomfort. Some ingredients, like hyaluronic acid, may also promote healing and support tissue health. Moisturizers work best for mild to moderate symptoms. If symptoms are more severe, your provider may recommend adding vaginal estrogen or other hormonal options.
- Explore lubricants: Lubricants help reduce friction during sexual activity and relieve discomfort right away. They come in water-, silicone-, and oil-based forms. While all types can help, water-based lubricants are usually recommended because they tend to cause less irritation.
- Choose breathable clothes: Tight-fitting underwear and synthetic fabrics can trap heat and moisture, increasing irritation and discomfort. The American College of Obstetricians and Gynecologists (ACOG) recommends wearing breathable, looser-fitting clothing—especially cotton underwear—and avoiding prolonged time in damp items like swimsuits or workout clothes. These choices can help reduce friction and keep the vulva dry and more comfortable.
What to avoid:
- Smoking: Exposure to nicotine through smoking, vaping, hookah, and other forms is not just bad for your overall health; it can also affect your vulva and vagina. A 2021 study found that smoking increases the likelihood of losing tissue in your vagina (atrophy).
- Scented products: Although fruity soaps and sprays may smell nice, they can cause irritation by altering the normal vaginal pH. Unscented soaps and washes are just as effective at cleansing without the added risks. Stick to the basics and save the fragrances for other parts of your body.
- Avoid douching: The vagina is self-cleaning. Instead of douching, just use water. By letting the vagina clean itself, you can avoid inflammation like vaginitis.
What to eat to improve vaginal health
While food alone won’t reverse tissue thinning, your diet can play a supporting role in how you feel during menopause—especially when it comes to overall wellness. Eating well helps support hormone balance, a stable weight, and even the health of your vaginal tissues.
- Mediterranean-style whole-food diet: Think colorful fruits and veggies, whole grains, lean proteins (like fish or beans), and healthy fats (like olive oil and avocado). This style of eating is linked to healthier aging and fewer menopausal symptoms—including less vaginal dryness and irritation. Plus, it supports long-term weight management, which can help keep hormones more balanced.
- Protein, calcium, vitamin D, and omega-3s: These nutrients support tissue resilience, bone strength, and circulation—factors that contribute to healthier skin all over your body. Together, these nutrients help your skin and mucosal surfaces (including vaginal tissue) stay stronger and more hydrated.
- Fiber: Eating a fiber-rich, mostly plant-based diet supports gut health—and a healthy gut may help promote a healthier vaginal environment, too. It’s all connected.
- Probiotics and yogurt: As estrogen declines, the balance of protective bacteria in the vagina shifts, which can affect pH and contribute to GSM symptoms. Early research suggests that oral probiotics may help support vaginal tissue health. Foods like yogurt with live cultures, kefir, sauerkraut, and kimchi could help balance your gut and vaginal microbiome, though we’re still learning exactly how strong the connection is.
Exercise as a tool for menopause labia health
You probably already know that exercise is great for your heart, bones, and mood—but did you know it may also support your vulva and vaginal health?
A study found that a higher BMI can affect the vulvar microbiome, which plays a role in maintaining healthy tissues down there. Staying active helps improve blood flow to the vulva and vagina, which is important for keeping those tissues nourished—especially during and after menopause. The researchers suggest keeping your BMI below 30 for optimal vulvar health.
The best part is don’t need to go overboard to see benefits. Regular movement—like walking, dancing, or strength training—can help maintain a healthy weight and preserve lean muscle (which naturally declines during menopause). Plus, muscle burns more calories than fat, which supports weight management over time.
The American Heart Association recommends:
- 150 minutes of moderate activity (like brisk walking) or
- 75 minutes of vigorous activity (like running) each week
- Plus strength training at least twice a week
Here are some ideas for incorporating exercise into your daily routine.
Supplements for vaginal health during menopause
Many people explore natural or non-hormonal options to manage symptoms like dryness, itching, and irritation during menopause. While some treatments show promise, it’s important to know that not all are backed by strong research. Here’s a look at what we do know:
- Vitamin E: According to the International Menopause Society, vitamin E may help with symptoms like dryness and itching. It can be taken orally or used topically. Some studies, like this one, suggest short-term relief—but we still need more research to confirm how well it works and how much to use.
- Vitamin D: The evidence on vitamin D is also mixed. A systematic review found that higher doses (800 IU or more) might help improve vaginal tissue and pH—especially when used vaginally—but not all studies agree. Still, maintaining healthy vitamin D levels is good for overall wellness, and it may play a supportive role.
- Aloe vera: A small study found that aloe vera cream could help relieve vaginal dryness and improve tissue health. It even performed similarly to low-dose estrogen in some cases. Another study suggests aloe may support hydration, reduce inflammation, and improve comfort during sexual activity.
- Fenugreek vaginal cream: In a short study, a 5% fenugreek cream improved vaginal dryness and cell health compared to placebo. While helpful, its effects were milder than estrogen therapy.
- Aloe vera and hyaluronic acid gel blends: Some products combine aloe, hyaluronic acid, sea buckthorn oil, and glycogen. One study showed this type of blend helped reduce vaginal dryness, improve pH, and enhance comfort and sexual function over 12 weeks.
- Probiotics and soy-based phytoestrogens: Early research on combinations of probiotics and plant estrogens (like soy isoflavones) has been mixed. One clinical trial found that pairing the two helped improve vaginal pH, moisture, and epithelial integrity in postmenopausal women. Still, larger studies are needed to confirm long-term benefits and optimal formulations.
Frequently Asked Questions (FAQ) about labia minora changes
Can a dermatologist help with my vulva and vagina during menopause?
Some dermatologists are trained in using lasers that repair the skin. Laser therapies are an effective and safe innovation for improving labia minora thinning during menopause. But it’s expensive and is usually not covered by insurance.
What is the #1 treatment for a shrinking labia minora?
Estradiol cream is considered the most effective treatment for vulvovaginal health during and after menopause.
Can sex help improve labia minora thinning?
Yes! The Menopause Society explains that having regular sexual activity (alone or with a partner) can actually help with symptoms of menopause. A study found that vulvar pain, dryness, and irritation in women improved with increased sexual activity.
Does labia minora thinning cause itchiness during menopause?
Probably not, but they are connected. When woman “lose” their labia minora, it’s usually accompanied by other symptoms of menopause, like dry, itchy skin in the vulva and vagina.
The bottom line: How Noom + HRTRx can help
Changes to the labia minora during menopause—like thinning, dryness, or the appearance of “disappearing”—can feel confusing. But these shifts are a common result of declining estrogen levels. While they can affect both comfort and confidence, there are effective treatments.
The most evidence-backed option is low-dose vaginal estrogen therapy, which helps:
- Restore local estrogen levels
- Rebuild tissue thickness and elasticity
- Improve hydration and comfort
If you’re also experiencing body-wide symptoms like hot flashes or mood shifts, systemic HRT (like pills or patches) may be recommended alongside or instead of local treatment.
The key is to speak with your healthcare provider. With the right plan, you can support your vulvar health and start feeling more like yourself again.
Noom + HRTRx can help. If you qualify, Noom can prescribe options like patches, creams, gels, sprays, and/or pills to improve your overall health through menopause.