Anxiety is more than just feeling nervous before an important event or restless during a stressful week. Anxiety conditions are defined by excessive fear, worry, or apprehension that is difficult to control, persists for weeks or months, and interferes with daily life. Symptoms often include constant worry, irritability, difficulty concentrating, muscle tension, and sleep disturbances. For some, these symptoms can escalate to the point of panic attacks or avoidance behaviors that affect relationships, work, and daily functioning.
During perimenopause and menopause, hormonal changes can increase the likelihood of developing an anxiety condition or worsen existing symptoms. Estrogen influences neurotransmitters like serotonin and GABA, which help regulate mood and calm the nervous system. As levels decline, many women report new or intensified anxiety, sometimes for the first time in their lives. Research suggests that women in early perimenopause are up to twice as likely to develop anxiety or depression compared to other life stages, which makes it important to recognize the signs.
For mild symptoms, lifestyle changes—such as exercise, stress reduction, mind–body practices, and healthy sleep habits—can often provide relief. But for moderate to severe cases, or when symptoms feel unmanageable, medical treatment or therapy may be necessary.
When is it time to see a doctor? If anxiety is persistent, interferes with daily life, or is accompanied by depressive symptoms, it’s important to talk with a healthcare provider.
Menopause-related anxiety is a hormonally influenced condition that deserves attention and care. From how it feels day-to-day, to why it happens, to when it’s time to see a doctor, understanding the full picture can help you recognize symptoms early and find the right ways to manage them.
Understanding menopause anxiety
Anxiety during menopause is a common symptom of the menopausal transition, which is the period leading up to and including menopause. Although exact rates are unknown, women are 1.5 times more likely to develop an anxiety disorder during perimenopause compared to premenopause. And during menopause, anxiety is incredibly common; 53% of menopausal women report experiencing anxiety.
Research shows that anxiety can emerge, even in people with no prior history of an anxiety disorder. The experience can range from mild nervousness and worry to severe panic attacks.
Anxiety during menopause is often different from other types of anxiety. It’s uniquely influenced by hormonal fluctuations related to the menopause transition. Some experts believe that anxiety experienced during menopause should even be treated as a different condition than what people experience in other times of their lives. While the symptoms may be similar, because the underlying causes are different, women in menopause may seek different treatments.
Deciding when to seek professional help for anxiety is an important step. During the menopausal transition, these symptoms can be easily dismissed as “normal” or temporary. While some level of anxiety or mood fluctuation is common during perimenopause, it’s important to recognize when it has become a health problem that requires medical attention. The Anxiety and Depression Association of America recommends seeking out professional help when your feelings and fears interfere with daily life.
What anxiety symptoms are linked to menopause?
Research from the Study of Women’s Health Across the Nation (SWAN) suggests that anxiety during the menopausal transition often includes:
- Irritability and being more reactive or easily overwhelmed
- Persistent tension or nervousness, even without a clear trigger
- Sudden, unexplained fear or dread, or a sense of being anxious for no obvious reason
- Palpitations or heart racing, physical sensations that can reinforce anxious feelings
- Mood swings, including rapid shifts between calm, anxious, or low moods
- Difficulty concentrating, as persistent worry can cloud memory and focus
These symptoms often appear or intensify during perimenopause and postmenopause, especially for women who didn’t experience significant anxiety earlier in life. Additionally, frequent vasomotor symptoms such as hot flashes and night sweats significantly increase the risk of anxiety.
In which stage of menopause does anxiety show up?
While anxiety can occur at any point in someone’s life, the hormonal changes throughout the three stages of menopause can affect the likelihood. Let’s look at what happens during each stage:
- Perimenopause (can begin in the late 30s): As your body runs out of eggs, hormone levels, particularly estrogen, can fluctuate. Many people notice hot flashes, night sweats, or changes in body shape (like more weight around the belly). Research shows that the risk of depression and anxiety rises during perimenopause, and for many, this is when symptoms feel the strongest. In fact, women in early perimenopause often report higher levels of anxiety and depression than before it begins and after menopause..
- Menopause (average age of 51): Menopause is typically confirmed when you’ve gone 12 consecutive months without a menstrual period.
- Postmenopause: Once menopause has been reached, your hormones will level out at a new, lower baseline. While some symptoms ease up, research shows that depression and anxiety can still be common. This is especially true for people who continue to experience hot flashes or have a history of major depression. Other factors—like personality traits (such as being prone to worry) and stressful life events—can also raise vulnerability, making postmenopause another important time to pay attention to mental health.
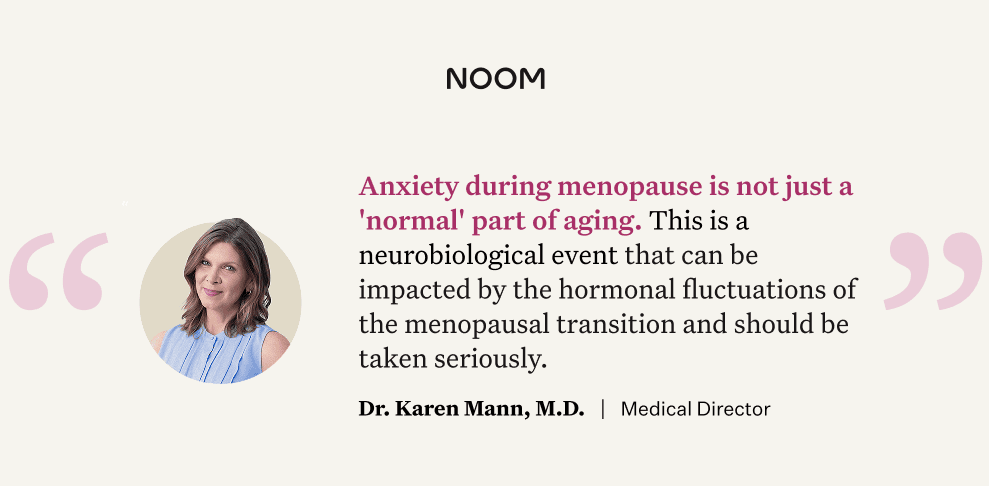
“The data really underscores that anxiety during menopause is not just a ‘normal’ part of aging. This is a neurobiological event,” says Dr. Karen Mann, MD, an OB-GYN and Noom Medical Director. “It’s important that doctors stop minimizing these symptoms as simply a consequence of aging or stress and instead recognize them for what they are. It’s a legitimate medical condition that can be impacted by the hormonal fluctuations of the menopausal transition and should be taken seriously.”
What causes anxiety during menopause?
There are a few key reasons why you might experience anxiety during menopause. Let’s break them down.
Hormones during menopause and anxiety
Estrogen does more than regulate your reproductive system—it also affects brain chemicals like serotonin, dopamine, and GABA, which help keep your mood steady, promote good sleep, and create a sense of calm. As estrogen levels drop during perimenopause, serotonin levels can fall too, often leading to irritability, nervousness, and anxiety. Lower estrogen also affects GABA, the brain’s natural “relaxation signal,” making it harder to cope with everyday stress.
At the same time, cortisol—your body’s main stress hormone—tends to rise with age. Higher cortisol can make you feel more on edge and can interfere with sleep, which only adds to feelings of anxiety. Together, these shifts in estrogen and cortisol can explain why so many women notice changes in mood during perimenopause and menopause.
Medical factors related to anxiety in menopause
A woman’s medical history can also be a strong predictor of how she experiences anxiety during perimenopause and menopause. Certain conditions and past medical history may make you more vulnerable, including:
- A history of major depressive disorder (MDD) – People who have struggled with depression in the past are at higher risk of experiencing mood disturbances again during this transition. The hormonal changes of menopause can sometimes trigger a recurrence of symptoms.
- Frequent hot flashes and night sweats – These vasomotor symptoms don’t just affect comfort; they can disrupt sleep, increase irritability, and worsen feelings of anxiety. Poor sleep in particular is a well-known contributor to mood problems.
- A history of PMS or PMDD – Women who have experienced significant mood swings tied to their menstrual cycles may be especially sensitive to the hormonal shifts of perimenopause.
How to reduce anxiety during menopause: Lifestyle changes
What you eat, how much you move your body, the quality of your sleep, and how you handle stress can all affect your mood. If you’re looking for natural remedies for menopause anxiety, many lifestyle changes can help you feel better.
Stress reduction to relieve anxiety in menopause
Research shows that mind–body practices such as tai chi, yoga, Pilates, and meditation can significantly ease anxiety during the menopausal transition. A study in the journal Menopause suggests that mind-body exercises can help relieve anxiety, depression, and fatigue in perimenopausal and postmenopausal women.
These practices seem to regulate the stress response, improve sleep, and bolster emotional resilience. Yoga and tai chi offer mindful movement combined with breath control, calming the nervous system; meditation enhances emotional regulation by reducing physiological stress markers; and Pilates improves body awareness and supports stress-reducing breathing.
How to use mind–body practices effectively for anxiety relief
- Prioritize consistency over duration. Studies found that regular engagement in mind–body exercises led to significant reductions in anxiety symptoms regardless of session length. This means that maintaining a steady routine matters more than worrying about the length of sessions.
- Start small with daily sessions. Even brief daily sessions—around 10–20 minutes—can meaningfully reduce anxiety symptoms over time.
- Make it sustainable and enjoyable. The positive outcomes seen in these studies are linked with long-term engagement. Practices that integrate smoothly into daily life—because they feel enjoyable and manageable—are easier to sustain and thus more likely to result in cumulative benefits.
- Pair with other healthy lifestyle strategies. Combining mind–body exercises with good sleep, balanced nutrition, and social support amplifies benefits. Studies show that improvements in mindfulness and mood regulation are tied to broader lifestyle improvements, including better sleep.
Sleep during menopause
Hot flashes and hormonal changes can make it harder to get restful sleep during menopause—and poor sleep can, in turn, worsen anxiety. A few simple strategies can help:
- Stick to a consistent sleep schedule – Going to bed and waking up at the same time every day helps regulate your body clock.
- Create a cool, dark sleep space – A cooler bedroom and blackout curtains or an eye mask can make it easier to stay asleep.
- Practice evening relaxation – Gentle yoga, meditation, or deep breathing can calm your mind before bed.
Even small adjustments can improve sleep quality and ease nighttime anxiety. For a full list of tips, see Menopause and Sleep: Common Issues and Expert-Backed Solutions.
Exercise to reduce anxiety during menopause
Studies show that exercise can improve mood and ease anxiety and depression during menopause. The key is consistency—regular activity tends to make the biggest difference. Here are a few approaches to consider:
- Aim for regular aerobic activity – Moderate-intensity exercise such as brisk walking, cycling, or swimming most days of the week has been shown to lower anxiety and depressive symptoms while boosting overall well-being.
- Incorporate resistance training – Strength work with weights, resistance bands, or bodyweight not only preserves bone and muscle mass but also helps regulate mood and build resilience.
- Try mind–body movement – Practices like yoga and tai chi combine movement with breathwork and mindfulness. This dual approach calms the nervous system, relieves stress, and improves sleep.
- Prioritize sustainability and enjoyment – The best exercise is the one you’ll stick with. Whether it’s a dance class, group fitness, or daily walks with a friend, choosing activities you enjoy makes them easier to maintain and more effective for managing anxiety long term.
How to eat to reduce anxiety during menopause
Adopting a balanced menopause-friendly diet means nourishing your body with a diverse, nutrient-rich mix of foods to support your changing physiology. This includes:
- Lean proteins, like as fish, chicken, eggs, tofu, or beans, are especially important during menopause to help maintain muscle mass, support bone health, and regulate hormones and neurotransmitters tied to mood and anxiety.
- Fruits and vegetables, which are packed with nutrients, have low caloric density, and contribute volume and satiety—making them a foundation for most meals and snacks.
- Fiber-rich complex carbohydrates, like whole grains and legumes, promote digestive health, steady energy, and fullness—key for mood stability and appetite control.
- Healthy fats, such as those found in fatty fish, avocado, olive oil, nuts, and seeds—added for heart and brain health, plus anti-inflammatory support during this hormonal transition.
This thoughtful mix forms the basis of a diet that not only supports healthy aging but also helps stabilize mood and anxiety during menopause.
- Magnesium-rich foods – Magnesium, often called the “relaxation mineral,” helps regulate neurotransmitters and lower cortisol. Good sources include leafy greens, pumpkin seeds, almonds, cashews, legumes, dark chocolate, and avocados.
- Foods with tryptophan – This amino acid is a precursor to serotonin, a neurotransmitter that supports mood and relaxation. Poultry, eggs, dairy, oats, nuts, and seeds are all rich in tryptophan.
When to see a doctor or mental health professional
Menopause can be a challenging journey, and it’s important to know when to seek help. While some anxiety is common, you should consider seeing a doctor or mental health professional if your menopause anxiety is persistent and interferes with your daily life. This includes difficulty sleeping, working, or maintaining relationships.
You should also seek professional help if you’re experiencing symptoms of depression, such as feelings of hopelessness, loss of interest in activities you once enjoyed, or suicidal thoughts. Remember, these professionals can help you understand what’s happening and guide you toward an effective treatment plan, whether it involves lifestyle changes, medication, or therapy.
Medical treatments for menopause anxiety
This could include hormone replacement therapy (HRT) to help manage hormonal imbalances, or medications that target mood and anxiety symptoms. These treatments can significantly improve quality of life when used as part of a comprehensive plan that may also include therapy and lifestyle support.
Medications that can help reduce anxiety
These options work by helping your brain regulate the neurotransmitters that affect your mood and stress levels. Common examples include:
- SSRIs (selective serotonin reuptake inhibitors): Medications like escitalopram (Lexapro) or paroxetine (Paxil) can help ease mood swings and hot flashes.
- SNRIs (serotonin-norepinephrine reuptake inhibitors): Venlafaxine (Effexor) is often used for hot flashes and may support energy and mental clarity by improving overall mood.
- Anti-anxiety medications (benzodiazepines) – Short-term use of medications such as lorazepam (Ativan) or clonazepam (Klonopin) may be considered for severe, acute anxiety. Because these can be habit-forming, they’re typically prescribed cautiously and for limited periods.
These treatments can be combined with talk therapy or counseling, which provide strategies for managing stress and navigating emotional challenges. For some women, a combination of medication, therapy, and lifestyle strategies works best.
How HRT can help with anxiety during menopause
HRT is often used off-label to treat menopause symptoms like anxiety by restoring the balance of hormones your body is no longer producing. HRT can be part of a comprehensive treatment plan for anxiety. When there are other clear signs of estrogen loss from someone’s age and other symptoms, this may be an option to consider.
There are two main types: estrogen-only HRT (for people who’ve had a hysterectomy) and combined estrogen–progestogen HRT (for those with a uterus, to reduce cancer risk). Both forms can help stabilize mood-related brain chemicals and ease anxiety.
Research supports its use: a recent study found that HRT can be effective in alleviating depressive and anxiety symptoms, particularly when hormone shifts are the underlying driver. And in some cases, combining HRT with mental health medications can deliver even greater relief. One meta-analysis reported that pairing SSRIs or SNRIs with HRT increased treatment efficacy to 92%, compared to just 48% with either approach alone. For women struggling with persistent anxiety, this combined strategy may make a meaningful difference in quality of life.
When to consider HRT: Experts generally recommend HRT for women who are under age 60 or within 10 years of menopause onset, since this is when the benefits tend to outweigh the risks. It may not be suitable for those with a history of certain cancers, cardiovascular disease, blood clots, or other contraindications. Talking with your healthcare provider about your personal health history and goals is the best way to determine if HRT is right for you.
“HRT is FDA-approved for managing vasomotor symptoms like flashes. For those who also have mood symptoms during their menopausal transition, HRT can help address both concerns,” says Dr. Mann. “For many women, HRT can be a straightforward, life-changing intervention that restores their sense of well-being and helps them feel like themselves again.”
For more details on how HRT works and the available options, see Exploring the Benefits of Hormone Replacement Therapy for Menopause.
FAQs about menopause and anxiety
When is anxiety most likely during menopause?
Perimenopause is often when women experience the highest rates of anxiety and mood changes. Hormone levels fluctuate dramatically during this time, creating what can feel like an emotional rollercoaster. Even people with no prior history of anxiety may notice symptoms.
Research shows that during perimenopause, women are 2 to 5 times more likely to develop a mood disorder and about 1.5 times more likely to develop issues related to anxiety. Anxiety is not only common, but often one of the earliest symptoms to appear. Women in perimenopause tend to report higher stress levels and more frequent anxiety than those who are postmenopausal.
Can menopause cause anxiety?
The hormonal fluctuations of perimenopause and menopause are a primary cause of increased anxiety. As estrogen and progesterone levels decline, they affect key neurotransmitters in your brain that regulate mood, leading to symptoms like irritability, nervousness, and dread.
What can I take for menopause anxiety?
For some, lifestyle changes like mindfulness, diet changes, exercise, and social support may be enough. For others, medical treatments like SSRIs, SNRIs, or hormone replacement therapy can be highly effective. The best approach is to talk to your doctor or a mental health professional to find a treatment plan that’s right for you.
How long does menopause anxiety last?
The duration of symptoms varies greatly from person to person. Anxiety is often most prevalent during the hormonal fluctuations of perimenopause. While it may decrease once hormone levels stabilize after menopause, for some people, anxiety can continue throughout the lifespan. The key is to manage your symptoms as they appear so you can feel better throughout your journey.
The bottom line: Managing anxiety during menopause
Menopause-related anxiety is common, but it is not something you have to simply “push through.” Hormonal shifts during this stage of life can disrupt brain chemistry, heighten stress responses, and trigger anxiety—even in women who have never experienced it before. The good news is that there are many effective strategies to manage symptoms, from lifestyle approaches like exercise, nutrition, sleep hygiene, and mind–body practices, to medical options including SSRIs, SNRIs, short-term anti-anxiety medications, and hormone replacement therapy (HRT).
What matters most is paying attention to your symptoms and seeking support. By combining healthy habits with professional care when needed, it’s possible to ease anxiety, improve mood, and feel more like yourself again. Menopause is a major life transition, but with the right tools and treatments, you can move through it with resilience, confidence, and peace of mind.
Looking for a more holistic way to navigate menopause? Noom + HRTRx could be the perfect fit. We’ll connect you with a qualified clinician who can help you explore HRT options, including patches and creams, to support your well-being. And because we know this journey is about more than just hormones, you’ll also get the Noom app and our expert-backed lessons to help you achieve your goals and find support.