What you’ll learn:
- Vaginal dryness after menopause happens mainly because lower estrogen makes vaginal tissue thinner, less elastic, and less capable of maintaining natural moisture.
- Mild dryness can often be managed with over-the-counter moisturizers and lubricants, but persistent symptoms may need prescription treatments like local HRT.
- Treating vaginal dryness early can help restore tissue health and prevent irritation or infections.
When your body reaches menopause, marked by going twelve months without a menstrual cycle, estrogen levels have dropped to a new, lower level. This hormonal shift can have different effects on your body. While hot flashes and weight gain are most commonly associated with menopause, there’s another cluster of symptoms called genitourinary syndrome of menopause (GSM) that can be very disruptive.
GSM includes symptoms like vaginal dryness, which might be accompanied by urinary urgency, painful urination, and even frequent urinary tract infections (UTIs). Studies show that symptoms affect an estimated 57% of postmenopausal women, and when you include related issues, the numbers are even higher.
Vaginal dryness can affect more than how your vagina feels—it can influence comfort during everyday activities and contribute to irritation that disrupts sleep. It can even increase the risk of infections. For those who are sexually active, it can cause pain during intercourse. Addressing dryness is important for protecting tissue health, preventing discomfort, and supporting overall quality of life.
Let’s talk about why (and when) you could experience vaginal dryness during menopause. We’ll talk about how you can manage dryness at home, when to reach out to your doctor, and explore whether hormone replacement therapy (HRT) or other medical treatments can help.
Vaginal dryness during menopause: What to expect
Before menopause, your ovaries produce lots of estrogen, a hormone with many important roles, including helping keep vaginal tissue moist, elastic, and healthy.
When estrogen levels drop after menopause, you may notice several dryness-related changes:
- Less natural stretch and moisture – With lower estrogen, the vaginal tissue produces less lubrication, making dryness more noticeable during everyday activities or intimacy.
- Thinning of the vaginal lining – Lower estrogen can make the tissue more delicate and prone to irritation or microtears, which can worsen dryness and discomfort.
- Changes in pH balance – Before menopause, beneficial bacteria help maintain a slightly acidic vaginal environment, which supports tissue health. After estrogen drops, the pH often rises, allowing protective bacteria to decline. This can increase the risk of infections, which may further aggravate dryness and irritation.
When vaginal dryness most often appears during menopause—and why the numbers vary
Vaginal dryness isn’t only a postmenopausal concern—it can begin earlier and often becomes more noticeable over time:
- Before menopause: Around 1 in 5 women report dryness, even before menopause, according to broader international surveys.
- One year post-menopause: Roughly 25% experience dryness at this stage.
- Three years post-menopause: Rates rise to about 47%.
- Later postmenopause: Larger, multi-site studies find between 44% and 57% of postmenopausal women report dryness, depending on how it’s defined and measured.
Across all peri- and postmenopausal stages: Some surveys suggest prevalence can range from 36% to nearly 90%, depending on population, symptom definitions, and methodology. These differences come down to study size, location, and how researchers define and measure dryness. What’s consistent is the takeaway: vaginal dryness is common, often increases after menopause, and—most importantly—it can be managed with the right strategies and support.
“These staggering numbers reveal that vaginal dryness is a common issue,” says Dr. Karen Mann, Noom Medical Director and OBGYN. “Although it may feel isolating, you are not alone, and there are options to feel better.”
Signs and symptoms of vaginal dryness during menopause
Vaginal dryness from genitourinary syndrome of menopause (GSM) can cause a range of physical, sexual, emotional, and urinary symptoms—many of which are connected through the same hormonal changes. Lower estrogen leads to thinner, less elastic tissue and reduced natural lubrication, which can impact comfort, sexual health, and urinary function.
Common symptoms include:
- Persistent feeling of dryness or lack of moisture – A constant or recurring sensation of dryness in the vaginal area, even without sexual activity.
- Itching, burning, or irritation – Dry tissue is more sensitive and can become irritated from everyday activities or clothing.
Pain or discomfort during sexual activity– Less lubrication and tissue fragility can make sexual activity uncomfortable or painful. - Light bleeding during or after sex – Fragile, dry tissue is more prone to small tears or microinjuries that cause spotting.
Increased sensitivity or tenderness – Dry, delicate tissue may feel sore or hypersensitive to touch.
“These symptoms can affect the entire body, and the effects of vaginal dryness aren’t just physical—they can deeply affect every part of your life,” says Dr. Mann.
When to see a doctor for vaginal dryness
Occasional dryness may improve with over-the-counter moisturizers or lubricants. But if the dryness is persistent, painful, or affecting your quality of life, it’s worth checking in with a healthcare provider.
You should also make an appointment if you notice itching, burning, bleeding, or pain during sex, since these can be signs of changes in the vaginal tissue that may need targeted treatment.
How vaginal dryness is diagnosed
The process starts with a conversation. Your healthcare provider will ask about your symptoms. Come prepared with the answers to these questions:
- How often do you feel dry?
- Does it affect daily comfort, intimacy, or activities like exercise?
- How much does it impact your quality of life?
They’ll also want to know about your menopausal status (natural, surgical, or medically induced) and whether you’ve noticed any related symptoms, such as irritation, itching, or urinary changes.
What to expect at your appointment
- A pelvic exam: An exam can help confirm what’s causing the dryness. During the exam, your provider may see signs that the vaginal tissue isn’t getting enough estrogen—such as pale, dry, or shiny walls; a loss of natural folds (rugae); or tissue that bleeds easily when touched. They might also notice petechiae (tiny red spots), redness, or thinning of the labia.
- In-office tests: Simple, in-office tests can also provide clues. One option is vaginal pH testing, which uses a small pH strip placed on the vaginal wall. A pH of 5.0 or higher suggests that the tissue has lost its protective acidity, which can happen when estrogen levels drop. Another is the Vaginal Health Index (VHI), which scores elasticity, moisture, epithelial integrity, fluid volume, and pH; lower scores can point toward dryness related to atrophy.
Because other conditions can cause dryness or irritation, your provider may also work to rule out issues like:
- yeast infections
- bacterial vaginosis
- skin conditions such as lichen sclerosus or lichen planus
- allergic reactions to soaps, detergents, or fabrics.
Sometimes, this means taking a sample of vaginal fluid to examine under a microscope. Blood tests for hormone levels aren’t considered useful for diagnosing vaginal dryness—they rarely add helpful information and aren’t part of standard care.
What you can do at home to manage vaginal dryness during menopause
The first step to finding relief from vaginal dryness is to avoid anything that makes it worse. Maintaining a healthy vagina and keeping the beneficial bacteria in balance can go a long way. Sometimes you don’t even need to add anything to your routine if you learn to care for the area gently. Here are some things to stop doing:
- Skip the scented soaps and washes: Avoid using soap, bath oils, or bubble baths around the vaginal area; rinsing the vulva with water is enough for cleansing.
- Use moisturizers: Regular use of vaginal moisturizers helps maintain moisture by directly nourishing the vaginal tissues.
- Use lubricants for sexual activity: To reduce dryness and discomfort during sexual activity, using a lubricant, especially one made with silicone, can provide additional relief.
- Avoid douching: This contributes to vaginal dryness and vaginitis
A guide to over-the-counter solutions
For women experiencing mild to moderate vaginal dryness, over-the-counter (OTC) products can be an effective and accessible first line of defense. However, the market is saturated with products whose formulations vary dramatically in quality and safety.
Making an informed choice means looking beyond brand recognition and understanding the science behind what makes a product helpful versus potentially harmful. It’s also important to know that these products aren’t regulated with the same rigor as prescription drugs, placing the burden of educated selection on the consumer.
Moisturizers vs. lubricants
The first step is knowing the difference between the two main categories: vaginal moisturizers and vaginal lubricants. They are not interchangeable—they’re designed for distinct purposes.
Vaginal moisturizers
Vaginal moisturizers are intended for regular, proactive use to manage ongoing, day-to-day dryness and discomfort.
- Purpose: Restore and maintain moisture within the vaginal tissues themselves by being absorbed into the skin and rehydrating the cells.
- Frequency of use: Apply every one to three days, regardless of sexual activity, for long-term comfort.
- Effect: Provide longer-lasting results than lubricants, aiming to improve the baseline health and hydration of the vaginal environment.
- Examples: Replens, Revaree, Luvena.
Vaginal lubricants
Vaginal lubricants are intended for on-demand use to make sexual activity more comfortable.
- Purpose: Coat the surface of the vulvar and vaginal tissues to reduce friction and pain during intercourse.
- Frequency of use: Apply immediately before or during sexual activity.
- Effect: Act quickly to provide short-term relief from discomfort, but don’t hydrate the tissues over time.
- Examples: K-Y, Astroglide, Sliquid.
| Feature | Vaginal moisturizers | Vaginal lubricants |
|---|---|---|
| Primary purpose | Provide ongoing hydration and restore moisture to vaginal tissues | Reduce friction and alleviate pain during sexual activity |
| Frequency of use | Regularly, every 1–3 days, regardless of sexual activity | On-demand, before or during sexual activity |
| How they work | Absorbed into the skin to rehydrate cells and improve baseline moisture | Coats tissue surfaces for temporary slipperiness and glide |
| How long they last | Longer-lasting, day-to-day comfort | Short-term, lasting for the duration of sexual activity. Silicone types typically last longer and are preferred. |
| Examples | Replens, Revaree, Luvena, Good Clean Love, Ah! Yes VM | K-Y, Astroglide, Sliquid, Slippery Stuff, Überlube, Pre-Seed |
The benefits of HRT and other medical treatments
If over-the-counter products aren’t enough—or if your symptoms are moderate to severe—prescription treatments can make a world of difference. These options have been developed with one goal in mind: target the tissues that need help, while minimizing unnecessary exposure or risks. The result? More choices than ever, even for women who were once told they couldn’t use hormone-based therapies.
Local estrogen therapy
Local, low-dose estrogen is considered the most effective treatment for genitourinary syndrome of menopause (GSM) because it treats the root cause: estrogen loss in vaginal tissues.
How it works: Unlike moisturizers that simply add hydration, local estrogen works at the cellular level. It stimulates the growth of vaginal epithelial cells, creating a thicker, more resilient lining. It improves blood flow, restores natural lubrication, and rebalances, bringing vaginal pH back to a healthy level. This not only relieves dryness and pain but can also lower your risk of urinary tract infections.
Forms to choose from (all equally effective):
- Vaginal creams (e.g., Estrace, Premarin) – Applied inside the vagina (and optionally on the vulva) daily at first, then 1–3 times per week for maintenance.
- Vaginal tablets or inserts (e.g., Vagifem, Imvexxy) – Small tablets or softgels placed high in the vagina, typically with a disposable applicator. Many find these less messy than creams.
- Vaginal ring (e.g., Estring) – A soft ring that stays in place for three months, releasing a steady, low dose of estrogen.
Safety profile: Because the dose is very low and applied locally, estrogen levels in the bloodstream generally stay within the normal postmenopausal range. That means:
- It doesn’t carry the same risks as higher-dose systemic hormone therapy.
- A progestin isn’t usually needed to protect the uterine lining.
- Even women with a history of hormone-sensitive breast cancer may be able to use it under oncology guidance if other options haven’t worked.
“If vaginal dryness is the primary concern, low-dose estradiol cream can often be used alone and has a great effect,” says Dr. Mann. “Sometimes, a combination of systemic and local HRT is the best approach.”
Systemic hormone therapy
If you’re experiencing GSM and other menopause symptoms—like hot flashes, night sweats, or mood changes—systemic HRT can be a comprehensive option. It works throughout the body to ease the full range of menopause symptoms.
Types of systemic HRT include:
- Oral tablets – Taken daily, containing estrogen alone or combined with a progestin.
- Transdermal patches – Deliver estrogen (and sometimes progestin) through the skin for steady hormone levels.
- Body creams – Topical treatments that deliver hormones through the skin
If you still have your uterus, systemic estrogen should be paired with progesterone to protect the uterine lining and lower the risk of endometrial cancer.
Even with systemic therapy, some women find they still need to add a local vaginal treatment for complete relief of GSM-related dryness and discomfort.
Non-hormonal options
- Ospemifene (Osphena) – This is an oral, non-estrogen prescription option. Ospemifene is a selective estrogen receptor modulator (SERM) that acts like estrogen in vaginal tissue—improving thickness, elasticity, and comfort—while avoiding stimulation of breast tissue and having minimal effect on the uterine lining. Taken as a 60 mg tablet daily with food, it’s approved for moderate to severe dyspareunia (pain during intercourse) due to GSM.
- Prasterone (Intrarosa) – A vaginal insert containing dehydroepiandrosterone (DHEA), a hormone precursor. Once inserted, DHEA is converted inside vaginal cells into small amounts of estrogen and androgens exactly where they’re needed, improving tissue health and moisture with minimal effect on hormone levels elsewhere in the body. Used nightly as a small wax-based insert, it’s prescribed for moderate to severe dyspareunia.
Lifestyle, nutrition, and complementary care for vaginal dryness
While medical treatments are the foundation for moderate-to-severe dryness and other genitourinary syndrome of menopause (GSM) symptoms, supportive strategies can improve comfort. These approaches work alongside—not instead of—medical care.
Lifestyle & daily habits
- Maintain regular sexual activity – Arousal increases pelvic blood flow, which nourishes vaginal tissues, stimulates moisture production, and helps maintain elasticity and tone.
- Quit smoking – Smoking reduces estrogen and narrows blood vessels, which worsens tissue thinning and dryness.
- Exercise and pelvic floor strengthening – Cardiovascular activity boosts circulation, while Kegels improve local blood flow and muscle tone, supporting vaginal tissue health.
- Avoid vulvar irritants – Again, harsh soaps, douching, and scented products can disrupt the balance of good bacteria in the vagina, strip protective oils, and aggravate dryness.
Nutrition & hydration
- Stay hydrated – Adequate hydration supports mucosal tissues, including the vaginal lining. Water-rich foods like cucumbers and watermelon also contribute to fluid intake.
- Adopt a menopause-supportive diet – Focus on lean proteins for muscle maintenance, fiber-rich produce for digestion, and healthy fats like omega-3s for anti-inflammatory benefits.
- Phytoestrogen-rich foods: Some foods, like soy, flaxseed, chickpeas, and lentils, contain plant compounds with mild estrogen-like activity. Meta-analyses suggest modest improvements in menopausal symptoms, including dryness, but the effects are generally small and vary by individual.
Stress management
- Incorporate stress-reduction practices – High cortisol can worsen hormonal imbalance. Techniques like yoga, meditation, deep breathing, and prioritizing sleep can improve tissue health and overall well-being.
The North American Menopause Society (NAMS) emphasizes that nonhormonal strategies—especially moisturizers, lubricants, and supportive lifestyle habits—are safe, effective, and important parts of a comprehensive care plan for vaginal dryness.
Complementary and natural options for vaginal dryness in menopause
For women seeking non-hormonal or natural ways to ease vaginal dryness, itching, or irritation, several topical and oral remedies show promise. Some are supported by strong clinical research, while others have only early or small-scale studies.
Hyaluronic acid
A powerful humectant that attracts and retains moisture, hyaluronic acid is available for vaginal use in suppositories and creams (e.g., Revaree). Multiple high-quality clinical studies show it can relieve dryness and improve tissue elasticity, with some results comparable to low-dose estrogen in mild cases—making it one of the most well-supported nonhormonal options.
Natural oils and gels
- Pure aloe vera gel: A water-based gel with soothing, hydrating, and anti-inflammatory properties. One randomized controlled trial found aloe vera cream to be as effective as prescription estrogen cream for relieving dryness, and another study suggests it may boost hydration and comfort during sex. While results are encouraging, the evidence base is still relatively small.
- Coconut oil: Smooth and long-lasting, coconut oil may help reduce friction and moisturize the vaginal area. Current evidence comes from a small pilot study using coconut oil paste, so more research is needed. Avoid if you have a coconut allergy, and note that oil-based products can damage latex condoms.
- Grape seed oil: A lightweight oil that absorbs quickly without greasy residue, grape seed oil may help moisturize and soothe irritated tissue. Some studies also point to its anti-inflammatory effects, but direct research on vaginal dryness is limited.
Vitamins and supplements
- Vitamin D: Research is mixed. Some trials suggest higher vaginal doses may improve tissue health and pH, but others show no significant benefit. At present, the evidence is not strong enough to recommend it as a primary treatment.
- Probiotics: Lactobacillus-containing probiotics, taken orally or vaginally, may help restore a healthy bacterial balance and support vaginal pH. Evidence in humans is still limited, so this remains a potential—rather than proven—supportive option.
Frequently asked questions (FAQ) about menopause and vaginal dryness
How long does vaginal dryness last?
Vaginal dryness is a chronic and progressive condition that typically begins after menopause and can last for years. Unlike other menopause symptoms that may improve over time, dryness won’t go away without treatment.
What’s the best lubricant for menopausal dryness?
The two main types are silicone and water-based lubricants. Silicone provides longer-lasting lubrication and is usually preferred for vaginal intercourse.
What are some other causes of vaginal dryness besides menopause?
Working with a healthcare provider is the best way to find out the reason behind your dryness and how to alleviate it. For example, it’s possible that allergy medications and antidepressants can also contribute to vaginal dryness.
The bottom line: Managing vaginal dryness during menopause
Vaginal dryness is one of the most common changes that happens after menopause. The main reason is lower estrogen. Without enough estrogen, the skin inside the vagina becomes thinner, less stretchy, and less able to hold moisture. Blood flow also drops, and the normal acidic pH changes. All of this makes the tissue drier and more likely to get irritated.
Treatment depends on how much it bothers you. For mild dryness, over-the-counter products like vaginal moisturizers and lubricants can help keep tissues comfortable and reduce pain during sex. If dryness is more severe—or if it doesn’t get better with these products—prescription options may be needed. These can include local estrogen therapy, systemic hormone therapy (combined with progestin if you have a uterus), or non-hormonal treatments like ospemifene or prasterone.
It’s worth talking to a healthcare provider early. The sooner vaginal dryness is treated, the easier it is to improve tissue health and prevent other problems, like irritation or infections.
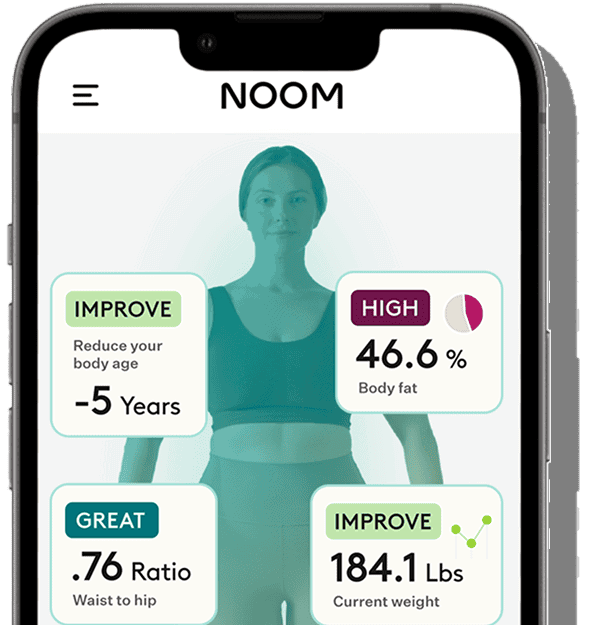
Noom + HRTRx can help you explore the options. If you’re eligible, you’ll be connected with a clinician who can prescribe HRT treatments like patches and creams to support your health throughout menopause. Plus, you’ll get access to Noom’s app along with proven behavior change lessons to help you lose weight and improve habits through menopause and beyond.